Hesi newborn with jaundice case study – HESI Newborn with Jaundice: A Comprehensive Case Study unveils a meticulously crafted exploration into the intricacies of neonatal jaundice, providing a profound understanding of its causes, manifestations, and management strategies.
This case study delves into the complexities of neonatal jaundice, examining its various etiologies, clinical presentations, and differential diagnoses. It illuminates the multifaceted nature of this condition, highlighting the essential role of comprehensive assessment and individualized treatment plans.
Neonatal Jaundice Overview
Neonatal jaundice is a common condition in newborns that causes the skin and whites of the eyes to turn yellow. It is caused by a build-up of bilirubin, a yellow pigment that is produced when red blood cells are broken down.
In most cases, neonatal jaundice is harmless and will go away on its own within a few weeks. However, in some cases, it can be a sign of a more serious underlying condition.
The causes of neonatal jaundice can be divided into two categories: physiological jaundice and pathological jaundice. Physiological jaundice is the most common type of neonatal jaundice and is caused by the normal breakdown of red blood cells in newborns. This type of jaundice usually appears within 2-3 days of birth and peaks at around 5-7 days.
It typically resolves on its own within 1-2 weeks.
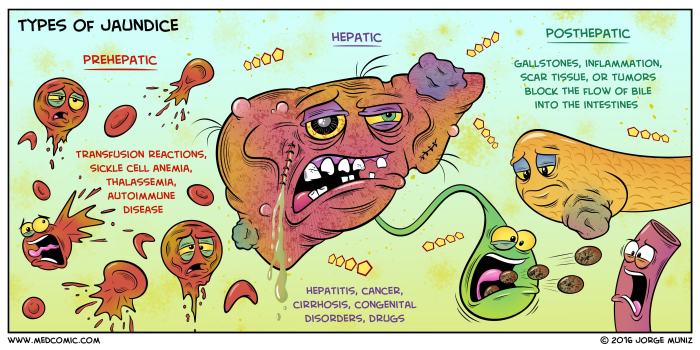
Pathological jaundice is caused by an underlying medical condition that prevents the liver from properly processing bilirubin. This type of jaundice can appear at any time during the first few weeks of life and can be more severe than physiological jaundice.
Some of the most common causes of pathological jaundice include:
- Biliary atresia
- Neonatal hepatitis
- Sepsis
- Hemolytic disease of the newborn
- Hypothyroidism
The clinical presentation of neonatal jaundice can vary depending on the severity of the condition. In mild cases, the skin and whites of the eyes may only be slightly yellow. In more severe cases, the skin and whites of the eyes may be deeply yellow and the baby may also have dark urine and pale stools.
HESI Case Study
A 3-day-old male infant is brought to the emergency department by his parents because of yellow skin and eyes. The infant was born at term via vaginal delivery and has been exclusively breastfed since birth. The infant is alert and active, and his vital signs are within normal limits.
On physical examination, the infant has jaundice of the skin and sclerae. The liver is palpable 2 cm below the costal margin and the spleen is not palpable. The infant’s abdomen is soft and non-tender.
Laboratory studies reveal a total bilirubin level of 15 mg/dL, a direct bilirubin level of 2 mg/dL, and an indirect bilirubin level of 13 mg/dL. The infant’s complete blood count and liver function tests are within normal limits.
The differential diagnosis for the infant’s jaundice includes:
- Physiological jaundice
- Breast milk jaundice
- Biliary atresia
- Neonatal hepatitis
- Sepsis
Management of Neonatal Jaundice
The treatment of neonatal jaundice depends on the severity of the condition. In mild cases, no treatment is necessary and the jaundice will resolve on its own within a few weeks. In more severe cases, treatment may include phototherapy or exchange transfusion.
Phototherapy is a treatment that uses ultraviolet light to break down bilirubin into a form that can be excreted by the body. Exchange transfusion is a procedure in which the infant’s blood is replaced with donor blood. This procedure is typically only used in cases of severe jaundice that is not responding to phototherapy.
Infants with neonatal jaundice should be monitored closely to ensure that the condition is not worsening. This may involve regular blood tests to measure bilirubin levels and physical examinations to assess the infant’s clinical status.
Nursing Care, Hesi newborn with jaundice case study
Nurses play an important role in the care of infants with neonatal jaundice. They can assess the infant’s condition, provide support to the family, and educate the family about the condition and its treatment.
When assessing an infant with neonatal jaundice, the nurse should:
- Inspect the infant’s skin and sclerae for yellowing.
- Palpate the infant’s liver and spleen.
- Assess the infant’s activity level and vital signs.
- Obtain a history from the parents about the infant’s feeding and elimination patterns.
The nurse can provide support to the family by:
- Explaining the condition and its treatment to the parents.
- Answering the parents’ questions and concerns.
- Providing reassurance and support to the parents.
The nurse can educate the family about the condition and its treatment by:
- Providing information about the causes and symptoms of neonatal jaundice.
- Explaining the different treatment options for neonatal jaundice.
- Teaching the parents how to care for their infant at home.
User Queries: Hesi Newborn With Jaundice Case Study
What are the common causes of neonatal jaundice?
Physiological jaundice, breast milk jaundice, and hemolytic jaundice are among the most prevalent causes.
How is neonatal jaundice diagnosed?
Diagnosis involves a thorough physical examination, laboratory tests (bilirubin levels), and assessment of risk factors.
What are the treatment options for neonatal jaundice?
Treatment modalities include phototherapy, exchange transfusion, and supportive care measures.
What is the role of nursing care in managing neonatal jaundice?
Nurses play a crucial role in monitoring infants, providing supportive care, and educating parents on the condition and its management.

